____
Should we consider giving nutrients like chlorella to clients seeking nutritional support before pregnancy – i.e., thinking more broadly than just omega-3s when it comes to water-based micronutrients?
YES. Absolutely. To start with: while supplements have been shown to be beneficial, they are not the same. Oils are triglycerides. The brain — and indeed all cell membranes throughout the body — use phosphoglycerides. It is important to understand there are two types of fat in the body:
(i) storage, as in round the waistline!
(ii) structural.
These contain the cell (plasma membrane) and the working structures of all cells in the body (e.g. the nuclear envelope and the energy-producing mitochondria). The membrane is a double layer of water-solubles on the outside and fatty acids on the inside, like a sandwich — which are water-insoluble — so separating the inside of the cell from the outside.
There are proteins embedded in these membranes that carry out many functions. However, the proteins are membrane-bound, so alteration of the fatty acids influences their function — hence explaining many effects of diet on health.
Cod liver oil, for example, is mainly triglycerides (storage fat). It contains 8% DHA and 12% EPA (a precursor of DHA). Cod muscle (which is what we eat) contains 47% DHA and very little EPA.
During early fetal development, neural cell division is occurring at the rate of over 1 million per second. Nature likes to use the preformed DHA rather than the long-winded process of synthesis.
So draw your own conclusions.
You spoke so passionately about the importance of a marine-based diet in supporting foetal brain development. Are there particular foods that offer superior nutritional value, or is it more about the overall benefits of fish, seafood, and seaweeds?
I think the answer is mostly given above.
The brain evolved in the sea 450 million years ago. DHA (docosahexaenoic acid) enters the scheme with the beginning of air-breathing life 600 million years ago, in things like the dinoflagellates — which we still have today. It captured UV photons, converting them into electrons, somewhat similar to what retinal does in our visible range today (DHA absorbs light in the UV, not our visible range).
There was no ozone layer 600 million years ago. The flow of electrons would have stimulated the evolution and growth of a nervous system, which became more and more needed as multicellularity evolved. The path of the electrons attracted and became surrounded by fatty layers — what we now call myelin — shielding the flow of electrons, eventually leading to the formation of complex systems like the eye of Orthoceras, and then the central nervous system and brain of the vertebrates 450 million years ago. (The cephalopods had different ideas — the octopus has several brains, needed for its eight tentacles, etc.)
The only stuff that nourished this progressive march of sophistication of the neural system was stuff from the sea.
Modern agriculture is running on trace-element-poor soils. There are over 2 million at risk of iodine deficiency, and its reappearance has been reported in UK schoolchildren:
Bath S, Rayman MP. Iodine deficiency in UK schoolgirls. Lancet. 2011 Nov 5;378(9803):1623; author reply 1624. doi: 10.1016/S0140-6736(11)61690-5. PMID: 22055035.
The other thing is — every time you eat a seafood meal, you have avoided eating the high sugar, high fat stuff of the modern commonality.
Many people have stopped eating marine foods due to concerns about heavy metals, microplastics, and marine pollution. What’s your perspective on this, and how can we balance the risks with the nutritional benefits?
Hibbeln JR, Spiller P, Brenna JT, Golding J, Holub BJ, Harris WS, Kris-Etherton P, Lands B, Connor SL, Myers G, Strain JJ, Crawford MA, Carlson SE. (2019) Relationships between seafood consumption during pregnancy and childhood and neurocognitive development: Two systematic reviews. Prostaglandins Leukot Essent Fatty Acids. 2019 Dec;151:14–36. doi: 10.1016/j.plefa.2019.10.002. PMID: 31739098.
Spiller P, Hibbeln JR, Myers G, Vannice G, Golding J, Crawford MA, Strain JJ, Connor SL, Brenna JT, Kris-Etherton P, Holub BJ, Harris WS, Lands B, McNamara RK, Tlusty MF, Salem N Jr, Carlson SE. (2019) An abundance of seafood consumption studies presents new opportunities to evaluate effects on neurocognitive development. Prostaglandins Leukot Essent Fatty Acids. 2019 Dec;151:8–13. doi: 10.1016/j.plefa.2019.10.001. PMID: 31669935.
This story comes from the US Food and Drug Administration, who did not do anything remotely like a research review of the science.
Without delving into the science as above, just think of Japanese women — they eat fish or seafood at most meals every day. They give birth to children who grow up to have the best longevity, the lowest rates of heart disease, the least common cancers, and the lowest incidence of major depression of any industrialised nation.
Where is the evidence of neurotoxicity?
There is none. It is some strange and suspicious motivation that led to this unscientific proclamation.
A study of 14,000 pregnancies in the Avon district assessed what women ate during pregnancy and followed the children born for eight years. After controlling for many confounders, this is what they found. Published in The Lancet by Joe Hibbeln and colleagues from Bristol, they also reported non-specific benefits to verbal reasoning power, motor skills, social skills, and behaviours — all positive.
The 2007 paper states that the FDA advisory will do harm — and that is exactly what it is doing.
Here is another data set showing what happens if the mother conforms to the FDA advisory.
Thank you for listening to me – buy our book The Shrinking Brain but read last 3 chapters first and the afterword! It is about all that stuff above!!
Best wishes
Michael

Should a child then stay on supplements for his whole life?
It depends on what is being treated – our experience is that, over time, the dose can be reduced, but symptoms can start reappearing if the treatment is stopped. If the diet is improved, then again, the need for extra nutrients is lessened.
Sadly, we live in a world of fast food and poorly remineralised soils, so ongoing additional nutrients can help support optimal functioning. Then, if you look at the research from David Smith’s group, you see that some extra B vitamins can slow cognitive decline – and so might be worthwhile continuing to supplement!
Also, life stages can increase our need for nutrients (more stress, pregnancy, teenage growth spurts, etc.), so that also influences our requirements.
Are the supplements available to buy in the UK?
Yes, I believe they are available through:
https://www.naturalmentalhealth.co.uk/products/daily-essential-nutrients
You can also try contacting them directly at: friends@naturalmentalhealth.co.uk
If that doesn’t work, then importing from the US is a viable option:
https://www.hardynutritionals.com/products/daily-essential-nutrients-360
What might have caused the high rates of diarrhoea noted when taking these micronutrients?
The nutrients definitely impact the microbiome (in a good way – we have published on this). I suspect that during the transition period, stools can become looser. One of the side effects of ultra-processed foods is constipation, so this is generally a good side effect! It usually resolves after a few weeks. Taking probiotics can help ease the transition, and increasing the dose more gradually also helps.
Please could you share details of the components of the “micronutrients” given in the trial mentioned?
Is there a single test you can take to check your vitamin and mineral levels, and where can you get it?
I’m not a big fan of testing, as I don’t think it highlights optimal needs.
Some people also ask about nutrient levels and whether they need to get theirs evaluated before trying micronutrients. We published a study showing that nutrient levels were not very good at predicting who would respond – and who wouldn’t – to treatment. Many people can have “normal” nutrient levels and still benefit from this approach.
We wonder if nutrient levels are only useful for identifying the nutritional needs of someone who is generally healthy. Perhaps those who are unwell – physically or mentally – have higher nutritional needs than the average person. If that’s the case, then nutrient testing may be of limited value in determining who might need more than what they can get from their diet.
Here are a few relevant papers:
I also wrote a blog on this topic, which you can read here:
https://blogs.canterbury.ac.nz/science/2018/11/30/should-i-get-my-nutrient-levels-checked-to-determine

Excellent information from Dr. Murphy regarding optimal rather than high levels of supplementation – does she have any guidelines on optimal supplementation rates?
Please see the table below, which I cut from the presentation for time:
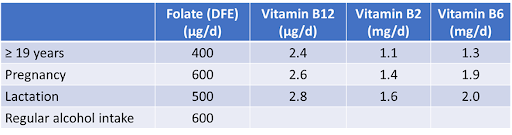
These are the guidelines from the IOM (USA).
For European guidelines, see: http://www.nap.edu/catalog/6015.html
Co-supplement with 2 µg/day of cyanocobalamin.
Remember that folic acid, along with other B vitamins and micronutrients, is added to fortified foods such as breakfast cereals in many countries. This contributes to meeting daily requirements.
In Europe, the availability of fortified foods varies according to regional legislation.
What test would she recommend to monitor B vitamin levels?
In the clinical setting, plasma/serum folate and cobalamin (vitamin B12) status are typically monitored using standard radioimmunoassays or protein-binding assays, depending on the provider and equipment available in the clinical lab.
Total homocysteine can also be measured. In fasting blood samples, it primarily reflects folate status, and secondarily cobalamin status – though it is also influenced by other nutrients and genetic factors involved in one-carbon metabolism.
Methylmalonic acid (MMA) is a specific functional marker of vitamin B12 deficiency. Holotranscobalamin (HoloTC), and the HoloTC/total cobalamin ratio, are interesting measures of the active form of vitamin B12 (indicating its availability for cellular uptake), although these are not routinely available.
In the research setting – particularly for assessing folate status – the gold standard method is the microbiological assay. Red blood cell folate status can also be measured. Total plasma/serum cobalamin can similarly be analysed via microbiological assay.
Functional assays for riboflavin (vitamin B2) and pyridoxine (vitamin B6), which involve measuring enzyme activity in erythrocytes, are considered gold standards. These include:
These functional assays require specific sample handling – including immediate processing on ice after collection – which makes them largely impractical for routine clinical use. Dedicated, specialised laboratories are required to perform these analyses, and I would very much like to see more of these become accessible!
What is the reference range for HCY and does it change with the age of the child?
This is a good question! There is more information available regarding reference ranges in adults. However, we have recently published reference ranges in pregnant mothers, for each trimester of pregnancy. There is a lot of data in the paper, including in the supplementary files. Please see:
Santos-Calderón LA, Cavallé-Busquets P, Ramos-Rodríguez C, Grifoll C, Rojas-Gómez A, Ballesteros M, Ueland PM, Murphy MM.
Folate and cobalamin status, indicators, modulators, interactions, and reference ranges from early pregnancy until birth: the Reus-Tarragona birth cohort study.
Am J Clin Nutr. 2024;120(5):1269–1283.
https://doi.org/10.1016/j.ajcnut.2024.09.015
PMID: 39326699
The article is free to download, and the relevant reference data can be found in the supplementary files.
Papandreou D, Mavromichalis I, Makedou A, Rousso I, Arvanitidou M.
Reference range of total serum homocysteine level and dietary indexes in healthy Greek schoolchildren aged 6–15 years.
Br J Nutr. 2006;96:719–24.
PMID: 17010232
Monsen AL, Refsum H, Markestad T, Ueland PM.
Cobalamin status and its biochemical markers methylmalonic acid and homocysteine in different age groups from 4 days to 19 years.
Clin Chem. 2003;49:2067–75.
DOI: 10.1373/clinchem.2003.019869
PMID: 14633879
Soldin OP, Dahlin JR, Gresham EG, King J, Soldin SJ.
IMMULITE 2000 age- and sex-specific reference intervals for alpha-fetoprotein, homocysteine, insulin, IGF-1, IGFBP-3, C-peptide, IgE, and intact parathyroid hormone.
Clin Biochem. 2008;41(12):937–42.
DOI: 10.1016/j.clinbiochem.2008.04.025
PMID: 18503765
Bailey D, Colantonio D, Kyriakopoulou L, Cohen AH, Chan MK, Armbruster D, Adeli K.
Marked biological variance in endocrine and biochemical markers in childhood: Establishment of paediatric reference intervals using healthy community children from the CALIPER cohort.
Clin Chem. 2013;59:1393–405.
DOI: 10.1373/clinchem.2013.204222
PMID: 23637247
Ganji V, Kafai MR.
Population references for plasma total homocysteine concentrations for U.S. children and adolescents in the post–folic acid fortification era.
J Nutr. 2005;135(9):2253–6.
DOI: 10.1093/jn/135.9.2253
PMID: 16140907
Do you believe there’s a need to shift public health messaging to emphasize not just folate intake, but also the quality and form – particularly the importance of using methylated folate and B12 for individuals who may carry genetic variants like MTHFR? Should this distinction be more strongly communicated in preconception care?
This is an interesting topic, but in my opinion, we’re not at this point yet from a public health perspective. Public health messages need to be simple and clear.
Yes, we can expect 5–20% of women (depending on the population) to have the MTHFR 677TT genotype, but the reality is that:
Generally, women of all genotypes – including those with the MTHFR 677TT variant – will benefit from supplementation with 400 µg/day of folic acid. The message needs to be:
“If there is a likelihood that you could become pregnant, you need to be taking 400 µg/day of folic acid.”
Adding conditions based on genotype or specific folate forms risks complicating this message and reducing its public health impact.
That said, replete riboflavin (vitamin B2) status is important in people with this genotype because the metabolic anomaly is caused by the partial dissociation of the FAD cofactor from the enzyme. The consequence is increased folate requirements, and folic acid supplementation can correct this.
Can Dr. Murphy share any studies comparing supplementation with folic acid versus methylfolate? Does she have any data on individuals with the DHFR genetic variation and their response to folic acid or methylfolate supplementation?
I’m afraid I have little information in this regard. We looked at the DHFR 19bp ins-del polymorphism in an adult population study. The homozygous variant genotype affected 19% of the population but was not associated with impaired folate status.
This was a randomly selected, age- and sex-stratified population sample representative of the adult population. Participants were non-users of B vitamin supplements, which was an eligibility requirement for participation.
For more detail, see:
Bueno O, Molloy AM, Fernandez-Ballart JD, García-Minguillán CJ, Ceruelo S, Ríos L, Ueland PM, Meyer K, Murphy MM.
Common polymorphisms that affect folate transport or metabolism modify the effect of the MTHFR 677C > T polymorphism on folate status.
J Nutr. 2016;146(1):1–8.
DOI: 10.3945/jn.115.223685
PMID: 26561410
What quantities of B12 particularly are safe – so many multis have high levels. Also what are ideal levels of Serum B12 and folate?
Vitamin B12 Supplementation: Clinical Considerations
Vitamin supplements containing 2 µg of B12 are safe when supplementation is used to prevent deficiency. However, treating a deficiency is a different matter. If oral administration is used (rather than intramuscular injections), significantly higher doses are generally required to achieve therapeutic effects – particularly in individuals with absorption issues.
It’s also important to consider whether patients are on medications such as metformin, which can interfere with B12 absorption. While few studies have investigated potential hypervitaminosis from high-dose B12 supplementation, some adverse effects have been reported.
Ideal Serum Levels for B12 and Folate
This remains an open question. While there are established deficiency thresholds, we still lack consensus on what constitutes optimal serum levels of B12 and folate for long-term health or disease prevention.
In short, more research is needed, particularly around:
Unfortunately, there is still a general misconception that B12 deficiency is mainly limited to India, Nepal, vegetarians, or older adults – which continues to hinder widespread awareness and screening.
For further reading, I recommend the work of:
Reference Ranges for Methylmalonic Acid
Mineva EM, Sternberg MR, Zhang M, et al.
Age-specific reference ranges are needed to interpret serum methylmalonic acid concentrations in the US population.
Am J Clin Nutr. 2019;110(1):158–168.
https://doi.org/10.1093/ajcn/nqz045
PMID: 31127807
Pregnancy Reference Ranges
Santos-Calderón LA, Cavallé-Busquets P, Ramos-Rodríguez C, et al.
Folate and cobalamin status, indicators, modulators, interactions, and reference ranges from early pregnancy until birth: the Reus-Tarragona birth cohort study.
Am J Clin Nutr. 2024;120(5):1269–1283.
https://doi.org/10.1016/j.ajcnut.2024.09.015
PMID: 39326699
British Committee for Standards in Haematology Guidelines
Devalia V, Hamilton MS, Molloy AM.
Guidelines for the diagnosis and treatment of cobalamin and folate disorders.
Br J Haematol. 2014;166(4):496–513.
https://doi.org/10.1111/bjh.12959
PMID: 24942828
WHO Guideline: Optimal Serum and RBC Folate Concentrations
Molloy AM and WHO
For the prevention of neural tube defects in women of reproductive age.
https://www.who.int/publications/i/item/9789241549042


When an autistic teenager is suffering from ARFID and eats too much sugary food, the temptation is to let them eat it because it is still calories. How can you help them move away from sugary foods, especially when they are demand avoidant? I have another child who is not ASD and she happily eats a well-balanced diet.
For those children who have a white diet/bland, and are addicted to the sugars and carbs in the foods, how is it best to introduce new foods when the idea of something new to the child results in..
This is a deeply important and very real challenge, especially common in children and
teenagers of all ages with sensory sensitivities, autism spectrum disorder (ASD), or ARFID
(Avoidant/Restrictive Food Intake Disorder). When children have a predominantly white,
bland, high-carb diet (like pasta, bread, chips, sugary yoghurts), it’s usually a combination of
sensory preferences, emotional regulation, and biological reward loops tied to processed
food.
Understanding the “Addiction” to Ultra-Processed Foods
– Carbs and sugar stimulate dopamine release, offering comfort and pleasure.
– Many white foods are also predictable in texture, colour, and taste, which is
reassuring for kids with anxiety or sensory issues.
– Trying a new food could be perceived as a real threat, not a mild inconvenience.
Here are some Evidence-Based Strategies for Expanding a Limited Diet
o Move in small, predictable steps.
o Remove ultra-processed foods slowly—otherwise, it may cause distress and
reduce trust.
o Replace sugary snacks with homemade versions with slightly better
ingredients. For example: Replace sugary yoghurt with plain Greek yoghurt
mixed with fruit puree.
5. Involve the Child in Choices
o Even small decisions (“Do you want your apple whole or sliced?”) give them a
sense of control.
o Involving them in shopping or prepping food can increase curiosity.
6. Consistent Routine
o Keep mealtimes and food options predictable. Many kids eat better when their
anxiety is reduced by routine.
Do you have any tips specifically for neurodiverse children, particularly around issues with textures and impulsivity?
In my experience with neurodivergent children – which it seems could cover many kids today -extreme reaction to textures or impulsivity varies. For example, an ASD child normally
would be much more resistant to many different textures than a child with ADHD. Whereas
an ADHD child may be more impulsive.
There may be no easy answer of course, but the most common textures that kids may reject
include slimy, lumpy or mashed or mushy. I need to add, that many children and adults who
have not been diagnosed as neurodiverse have textures issues and have had since young
children. This is something that I have not seen all people outgrow. ASD children typically
are much more sensitive to foods and it can be a challenge for many parents.
Key strategies include:
– Offering a variety of textures
– Avoiding known dislikes
– Using small portions
– Repeatedly offering new foods without giving in to unhealthy choices.
– For very resistant eaters (excluding extreme cases), skipping a meal without
alternatives can encourage trying accepted foods later.
In my years as a teacher and then as a doctor I have seen the impulsivity more in children
that have the hyperactive component of ADHD. A common situation would be an impulsive
child might blurt something out in class, or interrupt others when speaking. This impulse is
difficult and often impossible to control but overtime with help from adults a child can learn to
monitor it somewhat. As someone who has lived with ADHD for 78 years, I find myself
apologizing ‘sorry I didn’t mean to interrupt’ even now. Children can be taught to
acknowledge their impulsivity and if they many have offended someone, then apologize. In
my experience the impulsivity does not go away but it can be tamed.
In my experience, unless the child with ADHD or version of, is really struggling with school or
university, medication is not necessary. Awareness of the parents, teachers of the child
themselves can help create surroundings to help them focus.
Here are some tips that may help with impulsivity and other characteristics of ADHD, ASD
and other conditions that are considered to be neurodivergent:
Avoid or minimize exposure to:
– Food additives such as artificial colouring, like red dye #4, environmental toxins,
Electromagnetic Radiation, gluten (if sensitive), and excess sugar.
Nutrient support to consider:
– Omega-3 fatty acids are essential nutrients and necessary for a proper brain function
and development.
– Multivitamin: studies have shown that healthy children aged 8–14 given a daily
multivitamin and mineral supplement had increased accuracy in attention-based
tasks after only a few weeks
– Mineral deficiencies such as zinc, and magnesium have been shown to contribute to
ADHD, other learning disorders and ASD.
– Iron deficiency can cause a wide range of behavioural challenges and is commonly
found in those with ADHD. – Adolescents have higher iron requirements in order to
support rapid growth. Diet is often inadequate, especially in vegetarians.
– Protein – hyperactive children who ate a meal high in protein in the morning and or at
lunch did equally well or sometimes better in school than non-hyperactive kids.
Caregiver tips and strategies:
– Create structure, consistent routines, and reduce distractions.
– Break tasks into small steps, promote physical activity, and use positive
reinforcement.
– Educate those around the child to foster empathy and understanding.
– Support from counselling or CBT may be beneficial when needed.
Most supplements available state that they are suitable for children 2 or 3 years or older. However, ASD is frequently diagnosed at around age 2, and toddlers and small children often have very limited nutrition in their diets. My question would be: are there supplements that would be suitable for the weaning baby/toddler?
While many supplements are labelled for children aged 2 or 3 and above, there are
indeed options suitable for younger children, including those under 2 years old.
In the UK, all children aged 6 months to 5 years are recommended to take daily
vitamin supplements containing vitamins A, C, and D, unless they consume more
than 500ml of infant formula daily, which is already fortified with these vitamins. For
breastfed infants, a daily vitamin D supplement of 8.5 to 10 micrograms is
recommended from birth to 1 year of age. You can find supplement
recommendations for Smart Kids at Food for the Brain
https://foodforthebrain.org/smartkidssupplements/.
Considerations for Children with ASD
Children with ASD may have specific nutritional needs due to selective eating habits
or metabolic differences. Common deficiencies in children with ASD include Vitamin
D, Vitamin B12 and Folate (B9), Iron and Omega-3 Fatty Acids.
Tips for Supplementing Young Children
– Consult Healthcare Providers: Always discuss with a healthcare professional
before introducing new supplements.
– Check Age Appropriateness: Ensure the supplement is suitable for your child’s age
group.
– Monitor for Allergens: Be aware of any potential allergens in supplement
ingredients.
– Maintain a Balanced Diet:
How can we assess the quality of the vitamins/minerals we are buying? What would let us know we are buying good quality? I am using British Supplements as they say they are ‘clean’, but I have no idea!!!
Here are some tips on how to Assess the Quality of Vitamins and Minerals:
Examine the Ingredients List
o Avoid unnecessary additives like:
– Artificial colours and flavours
– High levels of added sugar or sugar alcohols
– Fillers and binders (e.g., magnesium stearate, titanium dioxide)
Review the Manufacturer’s Transparency
o Good brands often:
– Provide batch testing results or Certificates of Analysis (CoA)
– Clearly state country of origin and manufacturing practices
– Offer contact info for questions
Check for GMP Compliance
o Look for mention of GMP (Good Manufacturing Practices) compliance on the
label or website.
o GMP facilities are regularly inspected and held to higher standards for
hygiene, quality, and labelling.
I’ve noticed that some of the Children’s vitamins have added sugar. Where can you buy them that might be suitable for children but also palatable?
Here are some top tips for choosing low sugar vitamins for children
– Read the labels carefully: Look for added sugar amounts and terms like “cane sugar,”
“glucose syrup,” or “fruit juice concentrate.”
– Choose sugar-free or low-sugar options: Brands that use stevia, monk fruit, or xylitol
can offer a sweeter taste without spiking blood sugar.
– Stick to liquid or powder forms: These often have fewer additives and can be mixed
into food or drink without the sugary coating.
You can find supplement recommendations for Smart Kids at Food for the Brain
https://foodforthebrain.org/smartkidssupplements/.
Lots of evidence suggests that vitamin D is depleted during illness & I think also during operations & cancer treatment, so it’s recommended that we supplement with vitamin D (or calcifediol), but are there any other foods/supplements that should be taken during illnesses? Omega 3/6s, for example?
Vitamin D plays a crucial role in immune function, and its supplementation is recommended
before, during and after periods of illness. Beyond vitamin D, there are several other
nutrients and foods to support the body during illness:
Glutamine
Glutamine is an amino acid that supports gut health and immune function during
periods of stress or illness, when the body’s demand for glutamine may increase.
Vitamin C and Zinc
Vitamin C and zinc work in synergy in supporting immune health. These nutrients are
known to enhance the body’s defense mechanisms, particularly during infections and
recovery periods.
Omega-3 and Omega-6 Fatty Acids
Essential fatty acids, particularly omega-3s, are recommended for their anti-
inflammatory properties and role in maintaining cellular health. A balanced intake of
omega-3 and omega-6 fatty acids can aid in recovery and overall well-being during
illness.
Multivitamins and Minerals
A comprehensive multivitamin and mineral supplement can help address potential
deficiencies and support the body’s nutritional needs during illness.
A diet rich in the following whole foods can support recovery:
– Whole Grains and Legumes: Provide essential nutrients and fibre.
– Fresh Fruits and Vegetables: Offer a range of vitamins, minerals, and antioxidants.
– Nuts and Seeds: Supply healthy fats and protein.
– Oily Fish: Such as salmon and mackerel, are good sources of omega-3 fatty acids.
Food for the Brain offer at home finger prick blood tests, testing levels of Vitamin D,
Antioxidant Glutathione Index, Homoysteine, HbA1c (sugar control) and Omega 3 Index –
https://foodforthebrain.org/tests/.

Are there any further details available on what was used for chelation in the case with a 24:1 better-to-worse ratio? Was this intervention beyond the use of Epsom salt baths for detoxification?
I would recommend addressing the question to the Autism Research Institute which has published the report. https://autism.org/
I’d be interested in learning more about other chelation or binding interventions that were used, if that information is available.
Chelation is not a BANT approved procedure and I did not discuss the intervention.
What was used for chelation, please? Was it fulvic acid, humic acid, or another agent?
See above- I use fulvic/ humic acid for gut support mostly rather than chelation purposes.
Do you have any practitioner support resources for practitioners specialised in autism, such as group supervisory meetings or mentorship options?
Not at the moment, but I could look into these options – perhaps interested parties can contact me directly. There is a huge demand to support children with autism. I have more work than I can manage.
Which is the test for folate receptor antibodies, please?
I recommend that families contact Red Laboratories in Belgium, who can arrange shipment to Professor Ramaekers’s lab in the US. More information is available here:
https://www.redlabs.com/2022/03/autism-awareness-day-importance-of-frat.html
All folate supplements need to be discontinued for two weeks prior to the test.
A sample of 6–8 ml serum is required (centrifugation needed), and the sample must be frozen and shipped on ice.
Any experience and benefits of using supplements and interventions to increase BDNF in ASD kids, including: Lion’s mane mushroom, VCO/MCT oils, DHA omega-3 / I use this of course with EPA, Curcumin, IR sauna and Infrared light (PBM)?
Yes, these are all good options. Other approaches that may help increase BDNF include:
I don’t personally measure BDNF, so this is based on the published evidence, as well as knowledge shared at conferences and among other practitioners – all pointing to the potential benefit of these interventions.

Can neurotransmitters produced in the gut really affect brain neurotransmitters involved in brain regulation? I had thought gut neurotransmitters couldn’t influence brain neurotransmission directly.
While many neurotransmitters are synthesised in the gut, several of them do not cross the blood–brain barrier — including serotonin, glutamate, GABA, dopamine, and acetylcholine in most cases.
For example: serotonin produced in the gut cannot pass the barrier, although its precursor, tryptophan, can.
However, the neurotransmitter synthesis pathway in the intestine directly or indirectly influences brain activity and cognitive function. Short-chain fatty acids, neurotransmitters, and their precursors can affect the levels of related metabolites in the brain via the bloodstream, thereby regulating brain functions and cognition.
The gut–brain axis is a bi-directional system of communication.
In terms of vitamin D supplementation, what are the speaker’s thoughts on BetterYou oral sprays versus capsules taken with a fat-containing meal?
In my personal experience, I prefer gel capsules containing vitamin D₃, often combined with linseed (flax) oil. For children who cannot swallow capsules, a spray is probably a better option.
Regardless of the form, vitamin D should ideally be taken with a fatty meal or food to support absorption.
You say that stress increases the risk for ADD and ASD, but these are conditions present from birth – can you clarify?
This is a big question, and I’ll attempt to condense.
ADHD is usually diagnosed in childhood, and the heritability rate is about 80% – higher than most other mental health conditions. Children of parents with ADHD are 50% more likely to develop the condition; however, a parent having ADHD does not necessarily mean a child will develop it.
As with many gene variants associated with specific diseases or conditions, the presence of the variant increases the risk, but does not guarantee that the condition will manifest. The gene typically needs a trigger to become activated.
This is where epigenetics plays a role: environmental factors, lifestyle choices, and stress can all increase the risk of a genetic predisposition developing into an actual condition.
Epigenetics refers to how behaviours and the environment influence gene expression – that is, how genes are turned “on” or “off”.
DNA is the molecule that carries genetic information. A gene is a segment of DNA that contains instructions for making specific proteins.
Epigenetic changes do not alter the DNA sequence itself but affect whether or how much of a protein is made. These changes are typically reversible.
In contrast, some genetic disorders are caused by mutations in the DNA sequence, and these mutations are not reversible.
For example:
If autism spectrum disorder (ASD) were strictly the result of irreversible mutations in DNA, then recent reports showing reversal of symptoms through diet, lifestyle interventions, and targeted supplementation would not be possible.
A relevant case study:
D’Adamo CR, Nelson JL, Miller SN, et al.
Reversal of Autism Symptoms among Dizygotic Twins through a Personalised Lifestyle and Environmental Modification Approach: A Case Report and Review of the Literature.
J Pers Med. 2024 Jun 15;14(6):641.
https://doi.org/10.3390/jpm14060641

Dr John Gannage – The Role of Anti-nutrients and Detoxification in Neurodivergence
1. John Gannage has lots of US based information in terms of heavy metals etc. Does this hold true for the UK too?
2. I would be interested in studies about negative effect of EMF’S on childrens developing brain’s? especially as children are increasingly exposed to wifi all day at school, and sometimes at home too. I turn off wifi when not in use,and always at night, and use ethernet plug, but some households leave wifi on 24/7 which is cause for concern
3. Is there a lab testing dental samples for toxin exposure please?
4. Is there a test you can take to check your exposure to these contaminants? Where can you get it done?
5. Have you ever seen major regression on EDTA (suppositories)?
Jonathan Haidt – The Anxious Generation – rolling back phone-based childhood
As a presentation follow-up, please check this resource page. It’s designed to help you take the next steps with confidence and clarity. You’ll find action guides, sample texts, petitions, and other practical tools to support parents, educators, and even young people in working together to create real change around this issue.